^
ClinistixTM is a registered trademark of Bayer Corporation.
TestapeTM is a registered trademark of Eli Lilly Company.
ClinitestTM is a registered trademark of Miles, Inc.
Rx only
Manufactured for:
North Brunswick, NJ 08902
Manufactured by: Antibiotice SA, lasi 707410, Romania
December 2015 ASL01-2015

^Description
Ampicillin and Sulbactam for Injection USP is an injectable antibacterial combination consisting of the semisynthetic antibacterial ampicillin sodium and the beta-lactamase inhibitor sulbactam sodium for intravenous and intramuscular administration.
Ampicillin sodium is derived from the penicillin nucleus, 6-aminopenicillanic acid. Chemically, it is monosodium (2S, 5R, 6R)-6-[(R)-2-amino-2-phenylacetamido]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo [3.2.0] heptane-2-carboxylate and has a molecular weight of 371.39. Its chemical formula is C16H18N3NaO4S. The structural formula is:
Sulbactam sodium is a derivative of the basic penicillin nucleus. Chemically, sulbactam sodium is sodium penicillinate sulfone; sodium (2S, 5R)-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo [3.2.0] heptane-2-carboxylate 4,4-dioxide. Its chemical formula is C8H10NNaO5Swith a molecular weight of 255.22. The structural formula is:
Ampicillin and Sulbactam for Injection, USP, ampicillin sodium/sulbactam sodium parenteral combination, is available as a white to off-white dry powder for reconstitution. Ampicillin and Sulbactam for Injection USP dry powder is freely soluble in aqueous diluents to yield pale yellow to yellow solutions containing ampicillin sodium and sulbactam sodium equivalent to 250 mg ampicillin per mL and 125 mg sulbactam per mL. The pH of the solutions is between 8.0 and 10.0.
Dilute solutions (up to 30 mg ampicillin and 15 mg sulbactam per mL) are essentially colorless to pale yellow. The pH of dilute solutions remains the same.
1.5 g of Ampicillin and Sulbactam for Injection USP (1 g ampicillin as the sodium salt plus 0.5 g sulbactam as the sodium salt) parenteral contains approximately 115 mg (5 mEq) of sodium.
3 g of Ampicillin and Sulbactam for Injection USP (2 g ampicillin as the sodium salt plus 1 g sulbactam as the sodium salt) parenteral contains approximately 230 mg (10 mEq) of sodium.


^Microbiology
Ampicillin is similar to benzyl penicillin in its bactericidal action against susceptible organisms during the stage of active multiplication. It acts through the inhibition of cell wall mucopeptide biosynthesis. Ampicillin has a broad spectrum of bactericidal activityagainst many gram-positive and gram-negative aerobic and anaerobic bacteria. (Ampicillin is, however, degraded by beta-lactamases and therefore the spectrum of activity does not normally include organisms which produce these enzymes.)
A wide range of beta-lactamases found in microorganisms resistant to penicillins and cephalosporins have been shown in biochemical studies with cell free bacterial systems to be irreversibly inhibited by sulbactam. Although sulbactam alone possesses little useful antibacterial activity except against the Neisseriaceae, whole organism studies have shown that sulbactam restores ampicillin activity against beta-lactamase producing strains. In particular, sulbactam has good inhibitory activity against the clinically important plasmid mediated beta-lactamases most frequently responsible for transferred drug resistance. Sulbactam has no effect on the activity of ampicillin against ampicillin susceptible strains.
The presence of sulbactam in the Ampicillin and Sulbactam for Injection formulation effectively extends the antibacterial spectrum of ampicillin to include many bacteria normally resistant to it and to other beta-lactam antibacterials. Thus, Ampicillin and Sulbactam possesses the properties of a broad-spectrum antibacterial and a beta-lactamase inhibitor.
While in vitro studies have demonstrated the susceptibility of most strains of the following organisms, clinical efficacy for infections other than those included in the INDICATIONS AND USAGE section has not been documented.
Gram-Positive Bacteria: Staphylococcus aureus (beta-lactamase and non-beta-lactamase producing), Staphylococcus epidermidis (beta-lactamase and non-beta-lactamase producing), Staphylococcus saprophyticus (beta-lactamase and non-beta-lactamase producing), Streptococcus faecalis1 (Enterococcus), Streptococcus pneumoniae1 (formerly D. pneumoniae), Streptococcus pyogenes1, Streptococcus viridans1.
Gram-Negative Bacteria: Hemophilus influenzae (beta-lactamase and non-beta-lactamase producing), Moraxella (Branhamella) catarrhalis (beta-lactamase and non-beta-lactamase producing), Escherichia coli (beta-lactamase and non-beta-lactamase producing), Klebsiella species (all known strains are beta-lactamase producing), Proteus mirabilis (beta-lactamase and non-beta-lactamase producing), Proteus vulgaris, Providencia rettgeri, Providencia stuartii, Morganella morganii, and Neisseria gonorrhoeae (beta-lactamase and non-beta- lactamase producing).
Anaerobes: Clostridium species1, Peptococcus species1, Peptostreptococcus species, Bacteroides species, including B. fragilis.
________
1These are not beta-lactamase producing strains and, therefore, are susceptible to ampicillin alone.
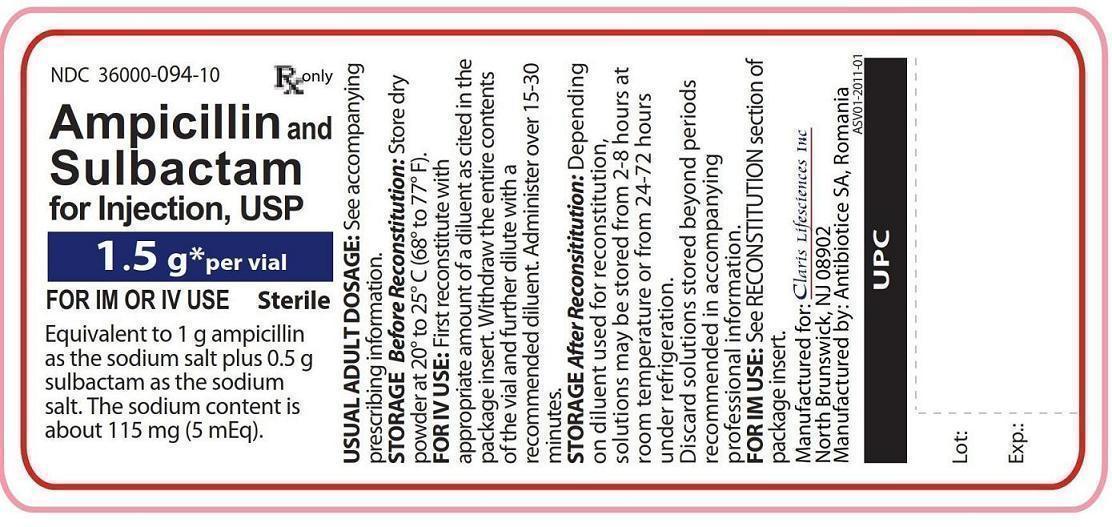
^Principal Display Panel - Gram Vial Label
NDC 36000-094-10 Rx only
Ampicillin and Sulbactam for Injection, USP
1.5 g* per vial
FOR IM OR IV USE Sterile
Equivalent to 1 g ampicillin as the sodium salt plus 0.5 g sulbactam as the sodium salt. The sodium content is about 115 mg(5 mEq).
^Diffusion Technique
For the disk diffusion method of susceptibility testing, a 20 mcg (10 mcg ampicillin + 10 mcg sulbactam) disk should be used. The standardized procedure1,2 requires the use of a standardized inoculum concentration. With this procedure, a report from the laboratory of “Susceptible” indicates that the infecting organism is likely to respond to Ampicillin and Sulbactam therapy and a report of “Resistant” indicates that the infecting organism is not likely to respond to therapy. An “Intermediate” susceptibility report suggests that the infecting organism would be susceptible to Ampicillin and Sulbactam if a higher dosage is used or if the infection is confined to tissues or fluids (e.g., urine) in which high antibacterial levels are attained.
^Preparation For Intravenous Use
Initially, the 1.5 grams and 3 grams vials may be reconstituted with Sterile Water for Injection to yield solutions containing 375 mg Ampicillin and Sulbactam per mL (250 mg ampicillin/125 mg sulbactam per mL).
An appropriate volume should then be immediately diluted with a suitable parenteral diluent to yield solutions containing 3 to 45 mg ampicillin and sulbactam for injection per mL (2 to 30 mg ampicillin/1 to 15 mg sulbactam/mL).
After the indicated time periods, any unused portions of solutions should be discarded.
TABLE 6:
^Directions For Use
General Dissolution Procedures: Ampicillin and Sulbactam for Injection USP, sterile powder for intravenous and intramuscular use, may be reconstituted with any of the compatible diluents described in this insert. Solutions should be allowed to stand after dissolution to allow any foaming to dissipate in order to permit visual inspection for complete solubilization.
^How Supplied
Ampicillin and Sulbactam for Injection USP (ampicillin sodium/sulbactam sodium) is supplied as a sterile white to off-white dry powder in glass vials. The following packages are available:
Vials containing 1.5 g (NDC 36000-094-10) equivalent of Ampicillin and Sulbactam for Injection, USP (1 g ampicillin as the sodium salt plus 0.5 g sulbactam as the sodium salt). 10 vials in a unit carton.
Vials containing 3 g (NDC 36000-095-10) equivalent of Ampicillin and Sulbactam for Injection, USP (2 g ampicillin as the sodium salt plus 1 g sulbactam as the sodium salt). 10 vials in a unit carton.
^Preparation For Intramuscular Injection
1.5 g and 3 g Vials: Vials for intramuscular use may be reconstituted with Sterile Water for Injection USP, 0.5% Lidocaine Hydrochloride Injection USP or 2% Lidocaine Hydrochloride Injection USP. Consult the following table for recommended volumes to be added to obtain solutions containing 375 mg Ampicillin and Sulbactam per mL (250 mg ampicillin/125 mg sulbactam per mL). Note: U se only freshly prepared solutions and administer within one hour after preparation.
TABLE 7:
*There is sufficient excess present to allow withdrawal and administration of the stated volumes.
^Indications And Usage
Ampicillin and Sulbactam for Injection, USP is indicated for the treatment of infections due to susceptible strains of the designated microorganisms in the conditions listed below.
Skin and Skin Structure Infections caused by beta-lactamase producing strains of Staphylococcus aureus, Escherichia coli,2 Klebsiella spp.2 (including K. pneumoniae2 ), Proteus mirabilis,2 Bacteroides fragilis,2 Enterobacter spp.,2 and Acinetobacter calcoaceticus.2
NOTE: For information on use in pediatric patients see PRECAUTIONS – Pediatric Use and CLINICAL STUDIES sections.
Intra-Abdominal Infections caused by beta-lactamase producing strains of Escherichia coli, Klebsiella spp. (including K. pneumoniae2 ), Bacteroides spp. (including B. fragilis), and Enterobacter spp.2
Gynecological Infections caused by beta-lactamase producing strains of Escherichia coli,2 and Bacteroides spp.2 (including B. fragilis2 ).
__________
2Efficacy for this microorganism in this organ system was studied in fewer than 10 infections.
While Ampicillin and Sulbactam for Injection USP is indicated only for the conditions listed above, infections caused by ampicillin susceptible organisms are also amenable to treatment with Ampicillin and Sulbactam for Injection USP due to its ampicillin content. Therefore, mixed infections caused by ampicillin-susceptible organisms and beta-lactamase producing organisms susceptible to Ampicillin and Sulbactam for Injection USP should not require the addition of another antibacterial.
Appropriate culture and susceptibility tests should be performed before treatment in order to isolate and identify the organisms causing infection and to determine their susceptibility to Ampicillin and Sulbactam.
Therapy may be instituted prior to obtaining the results from bacteriological and susceptibility studies, when there is reason to believe the infection may involve any of the beta-lactamase producing organisms listed above in the indicated organ systems. Once the results are known, therapy should be adjusted if appropriate.
To reduce the development of drug-resistant bacteria and maintain effectiveness of Ampicillin and Sulbactam and other antibacterial drugs, Ampicillin and Sulbactam for Injection USP should be used only to treat infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
^Principal Display Panel - 3 Gram Vial Label
NDC 36000-095-10 Rx only
Ampicillin and Sulbactam for Injection, USP
3 g* per vial
FOR IM OR IV USE Sterile
Equivalent to 2 g ampicillin as the sodium salt plus 1 g sulbactam as the sodium salt. The sodium content is about 230 mg(10 mEq).

^Adverse Reactions
Adult Patients: Ampicillin and Sulbactam is generally well tolerated. The following adverse reactions have been reported.
Local Adverse Reactions Pain at I.M. injection site – 16%Pain at I.V. injection site – 3%Thrombophlebitis – 3%Phlebitis – 1.2%
^Principal Display Panel - Gram Carton Label
NDC 36000-094-10 Rx only
Ampicillin and Sulbactam for Injection, USP
1.5 g* per vial
FOR IM OR IV USE Sterile
Equivalent to 1 g ampicillin as the sodium salt plus 0.5 g sulbactam as the sodium salt. The sodium content is about 115 mg(5 mEq).

^Contraindications
The use of Ampicillin and Sulbactam for Injection USP is contraindicated in individuals with a history of hypersensitivity reactions (e.g. anaphylaxis or Steven-Johnson syndrome) to ampicillin, sulbactam or to other beta-lactam antibacterial drugs (e.g. penicillins and cephalosporins).
Ampicillin and Sulbactam for Injection USP is contraindicated in patients with a previous history of cholestatic jaundice/hepatic dysfunction associated with Ampicillin and Sulbactam for Injection USP.
^Pregnancy
Pregnancy Category B: Reproduction studies have been performed in mice, rats, and rabbits at doses up to ten (10) times the human dose and have revealed no evidence of impaired fertility or harm to the fetus due to Ampicillin and Sulbactam. There are, however, no adequate and well controlled studies in pregnant women. Because animal reproduction studies are not always predictive of human response, this drug should be used during pregnancy only if clearly needed. (See – PRECAUTIONS - Drug/Laboratory Test Interactions section. )
^Dilution Techniques
Broth, agar, microdilution or equivalent methods may be used to determine the minimal inhibitory concentration (MIC) value for susceptibility of bacterial isolates using standardized methods, inoculums and concentrations of ampicillin/sulbactam.2,3,4
The recommended dilution method employs a constant ampicillin/sulbactam ratio of 2:1 in all tubes with increasing concentrations of ampicillin. MICs are reported in terms of ampicillin concentration in the presence of sulbactam at a constant 2 parts ampicillin to 1 part sulbactam.
TABLE 2: Recommended Ampicillin/Sulbactam, Disk Diffusion and MIC Susceptibility Ranges a,b,c (Zone Diameter in mm)
a The non-beta-lactamase producing organisms which are normally susceptible to ampicillin, such as Streptococci , will have similar zone sizes as for ampicillin disks.
b Staphylococci resistant to methicillin, oxacillin, or nafcillin must be considered resistant to Ampicillin and Sulbactam for Injection.
c The quality control cultures should have the following assigned daily ranges for ampicillin/ sulbactam (see Table 3):
TABLE 3: Quality control ranges for Ampicillin/sulbactam disk diffusion and MIC determinations
^Storage
Prior to reconstitution store dry powder at 20° to 25° C (68° to 77° F). [See USP controlled room temperature].
^References
^Principal Display Panel - 3 Gram Carton Label
NDC 36000-095-10 Rx only
Ampicillin and Sulbactam for Injection, USP
3 g* per vial
FOR IM OR IV USE Sterile
Equivalent to 2 g ampicillin as the sodium salt plus 1 g sulbactam as the sodium salt. The sodium content is about 230 mg(10 mEq).

^Precautions
General: A high percentage of patients with mononucleosis who receive ampicillin develop a skin rash. Thus, ampicillin class antibacterials should not be administered to patients with mononucleosis. In patients treated with Ampicillin and Sulbactam for Injection the possibility of superinfections with mycotic or bacterial pathogens should be kept in mind during therapy. If superinfections occur (usually involving Pseudomonas or Candida), the drug should be discontinued and/or appropriate therapy instituted.
Prescribing Ampicillin and Sulbactam for Injection in the absence of proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
^Warnings
Hypersensitivity SERIOUS AND OCCASIONALLY FATAL HYPERSENSITIVITY (ANAPHYLACTIC) REACTIONS HAVE BEEN REPORTED IN PATIENTS ON PENICILLIN THERAPY. THESE REACTIONS ARE MORE APT TO OCCUR IN INDIVIDUALS WITH A HISTORY OF PENICILLIN HYPERSENSITIVITY AND/ OR HYPERSENSITIVITY REACTIONS TO MULTIPLE ALLERGENS. THERE HAVE BEEN REPORTS OF INDIVIDUALS WITH A HISTORY OF PENICILLIN HYPERSENSITIVITY WHO HAVE EXPERIENCED SEVERE REACTIONS WHEN TREATED WITH CEPHALOSPORINS. BEFORE THERAPY WITH A PENICILLIN, CAREFUL INQUIRY SHOULD BE MADE CONCERNING PREVIOUS HYPERSENSITIVITY REACTIONS TO PENICILLINS, CEPHALOSPORINS, AND OTHER ALLERGENS. IF AN ALLERGIC REACTION OCCURS, AMPICILLIN AND SULBACTAM FOR INJECTION SHOULD BE DISCONTINUED AND THE APPROPRIATE THERAPY INSTITUTED.
Hepatotoxicity
Hepatic dysfunction, including hepatitis and cholestatic jaundice has been associated with the use of Ampicillin and sulbactam for injection. Hepatic toxicity is usually reversible; however, deaths have been reported. Hepatic function should be monitored at regular intervals in patients with hepatic impairment.
Clostridium difficile Associated Diarrhea: Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Ampicillin and Sulbactam, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibacterial drug use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibacterial drug use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibacterial treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.