^ Serious Asthma-related Events - Hospitalizations, Intubations, Deaths
^ Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling ( Patient Informationand Instructions for Use) with each new prescription and refill.
The complete text of the Patient Information is reprinted at the end of this document.Patients should be given the following information:
^ Description
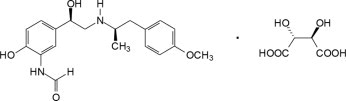
Arformoterol Tartrate Inhalation Solution is a sterile, clear, colorless, aqueous solution of the tartrate salt of arformoterol, the (R,R)-enantiomer of formoterol.
Arformoterol is a selective beta 2-adrenergic bronchodilator. The chemical name for arformoterol tartrate is formamide, N-[2-hydroxy-5-[(1R)-1-hydroxy-2-[[(1R)-2-(4-methoxyphenyl)-1-methylethyl]amino]ethyl]phenyl]-, (2R,3R)-2,3-dihydroxybutanedioate (1:1 salt), and its established structural formula is as follows:
The molecular weight of arformoterol tartrateis 494.5 g/mol, and its empirical formula is C 19H 24N 2O 4•C 4H 6O 6(1:1 salt). It is a white to off-white solid that is slightly soluble in water.
Arformoterol tartrate is the United States Adopted Name (USAN) for (R,R)-formoterol L-tartrate.
Arformoterol Tartrate Inhalation Solution is supplied as 2 mL of arformoterol tartrate solution packaged in 2.1 mL unit-dose, low-density polyethylene (LDPE) unit-dose vials. Each unit-dose vial contains 15 mcg of arformoterol (equivalent to 22 mcg of arformoterol tartrate) in a sterile, isotonic saline solution, pH-adjusted to 5.0 with citric acid and sodium citrate.
Arformoterol Tartrate Inhalation Solution requires no dilution before administration by nebulization. Like all other nebulized treatments, the amount delivered to the lungs will depend upon patient factors, the nebulizer used, and compressor performance. Using the PARI LC ®Plus nebulizer (with mouthpiece) connected to a PARI DURA NEB ™3000 compressor under in vitroconditions, the mean delivered dose from the mouthpiece (% nominal) was approximately 4.1 mcg (27.6%) at a mean flow rate of 3.3 L/min. The mean nebulization time was 6 minutes or less. Arformoterol Tartrate Inhalation Solution should be administered from a standard jet nebulizer at adequate flow rates via face mask or mouthpiece.
Patients should be carefully instructed on the correct use of this drug product (please refer to the accompanying Patient Information).
^ Cardiovascular Effects
Arformoterol Tartrate Inhalation Solution, like other beta 2-agonists, can produce a clinically significant cardiovascular effect in some patients as measured by increases in pulse rate, systolic and/or diastolic blood pressure, and/or symptoms. If such effects occur, the drug may need to be discontinued. In addition, beta-agonists have been reported to produce ECG changes, such as flattening of the T-wave, prolongation of the QTc interval, and ST segment depression. The clinical significance of these findings is unknown. Arformoterol Tartrate Inhalation Solution, as with other sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension.
^ Adrenergic Drugs
If additional adrenergic drugs are to be administered by any route, they should be used with caution because the sympathetic effects of arformoterol may be potentiated [ see Warnings and Precautions ( 5.3, 5.5, 5.6, 5.7) ].
^ Overdosage
The expected signs and symptoms associated with overdosage of Arformoterol Tartrate Inhalation Solution are those of excessive beta-adrenergic stimulation and/or occurrence or exaggeration of any of the signs and symptoms listed under ADVERSE REACTIONS. Signs and symptoms may include angina, hypertension or hypotension, tachycardia, with rates up to 200 beats/min, arrhythmias, nervousness, headache, tremor, dry mouth, palpitation, muscle cramps, nausea, dizziness, fatigue, malaise, hypokalemia, hyperglycemia, metabolic acidosis and insomnia. As with all inhaled sympathomimetic medications, cardiac arrest and even death may be associated with an overdose of Arformoterol Tartrate Inhalation Solution.
Treatment of overdosage consists of discontinuation of Arformoterol Tartrate Inhalation Solution together with institution of appropriate symptomatic and/or supportive therapy. The judicious use of a cardioselective beta-receptor blocker may be considered, bearing in mind that such medication can produce bronchospasm. There is insufficient evidence to determine if dialysis is beneficial for overdosage of Arformoterol Tartrate Inhalation Solution. Cardiac monitoring is recommended in cases of overdosage.
^ Paradoxical Bronchospasm
As with other inhaled beta 2-agonists, Arformoterol Tartrate Inhalation Solution can produce paradoxical bronchospasm that may be life-threatening. If paradoxical bronchospasm occurs, Arformoterol Tartrate Inhalation Solution should be discontinued immediately and alternative therapy instituted.
^ Hepatic Impairment
Arformoterol Tartrate Inhalation Solution should be used cautiously in patients with hepatic impairment due to increased systemic exposure in these patients [ see Clinical Pharmacology ( 12.3) ].
^ Adult Copd Trials
Arformoterol Tartrate Inhalation Solution was studied in two identical, 12-week, double-blind, placebo- and active-controlled, randomized, multi-center, parallel group trials conducted in the United States (Clinical Trial A and Clinical Trial B). A total of 1,456 adult patients (age range: 34 to 89 years; mean age: 63 years; gender: 860 males and 596 females) with COPD who had a mean FEV 1of 1.3 L (42% of predicted) were enrolled in the two clinical trials. The racial/ethnic distribution in these two trials included 1383 Caucasians, 49 Blacks, 10 Asians, and 10 Hispanics, and 4 patients classified as Other. The diagnosis of COPD was based on a prior clinical diagnosis of COPD, a smoking history (greater than 15 pack-years), age (at least 35 years), spirometry results (baseline FEV 1≤65% of predicted value and >0.70 L, and a FEV 1/forced vital capacity (FVC) ratio ≤70%). About 80% of patients in these studies had bronchodilator reversibility, defined as a 10% or greater increase in FEV 1after inhalation of 2 actuations (180 mcg racemic albuterol from a metered dose inhaler). Both trials compared Arformoterol Tartrate Inhalation Solution 15 mcg twice daily (288 patients), 25 mcg twice daily (292 patients), 50 mcg once daily (293 patients) with placebo (293 subjects). Both trials included salmeterol inhalation aerosol, 42 mcg twice daily as an active comparator (290 patients).
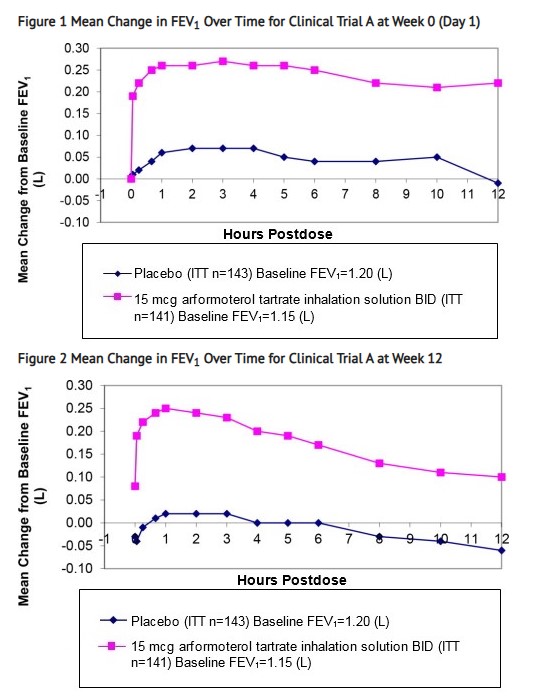
In both 12-week trials, Arformoterol Tartrate Inhalation Solution 15 mcg twice daily resulted in a statistically significant change of approximately 11% in mean FEV 1(as measured by percent change from study baseline FEV 1at the end of the dosing interval over the 12 weeks of treatment, the primary efficacy endpoint) compared to placebo. Compared to Arformoterol Tartrate Inhalation Solution 15 mcg twice daily, Arformoterol Tartrate Inhalation Solution 25 mcg twice daily and 50 mcg once daily did not provide sufficient additional benefit on a variety of endpoints, including FEV 1, to support the use of higher doses. Plots of the mean change in FEV 1values obtained over the 12 hours after dosing for the Arformoterol Tartrate Inhalation Solution 15 mcg twice daily dose group and for the placebo group are provided in Figure 1and 2 for Clinical Trial A, below. The plots include mean FEV 1change observed after the first dose and after 12 weeks of treatment. The results from Clinical Trial B were similar.
Arformoterol tartrate inhalation solution 15 mcg twice daily significantly improved bronchodilation compared to placebo over the 12 hours after dosing (FEV1 AUC0 to 12h). This improvement was maintained over the 12-week study period.
Following the first dose of arformoterol tartrate inhalation solution 15 mcg, the median time to onset of bronchodilation, defined by an FEV1 increase of 15%, occurred at 6.7 min. When defined as an increase in FEV1 of 12% and 200 mL, the time to onset of bronchodilation was 20 min after dosing. Peak bronchodilator effect was generally seen within 1 to 3 hours of dosing.
In both clinical trials, compared to placebo, patients treated with arformoterol tartrate inhalation solution demonstrated improvements in peak expiratory flow rates, supplemental ipratropium and rescue albuterol use.
^ Coexisting Conditions
Arformoterol Tartrate Inhalation Solution, like other sympathomimetic amines, should be used with caution in patients with cardiovascular disorders, especially coronary insufficiency, cardiac arrhythmias, and hypertension; in patients with convulsive disorders or thyrotoxicosis, and in patients who are unusually responsive to sympathomimetic amines. In two pooled, 12-week, placebo-controlled trials investigating Arformoterol Tartrate Inhalation Solution doses of 15 μg BID, 25 μg BID, and 50 μg QD, changes in mean predose and 2-hour post dose systolic and/or diastolic blood pressure were seen as a general fall of 2-4 mm/Hg; for pulse rate the mean of maximal increases were 8.8-12.0 beats/min. Over the course of a one-year study measuring serial electrocardiograms while receiving a dose of 50 mcg daily of Arformoterol Tartrate Inhalation Solution resulted in an approximately 3.0 ms increase in QT C-Fcompared to the active comparator, salmeterol. Doses of the related beta 2-agonist albuterol, when administered intravenously, have been reported to aggravate preexisting diabetes mellitus and ketoacidosis.
^3 Dosage Forms And Strengths
Arformoterol Tartrate Inhalation Solution is supplied as a sterile solution for nebulization in low-density polyethylene unit-dose vials. Each 2 mL vial contains 15 mcg of arformoterol equivalent to 22 mcg of arformoterol tartrate.
^ Pediatric Use
Arformoterol Tartrate Inhalation Solution is approved for use in the long-term maintenance treatment of bronchoconstriction associated with chronic obstructive pulmonary disease, including chronic bronchitis and emphysema. This disease does not occur in children. The safety and efficacy of Arformoterol Tartrate Inhalation Solution in pediatric patients have not been established.
^ Excessive Use Of Arformoterol Tartrate Inhalation Solution And Use With Other Long-acting Beta 2-agonists
Fatalities have been reported in association with excessive use of inhaled sympathomimetic drugs. As with other inhaled beta 2-adrenergic drugs, Arformoterol Tartrate Inhalation Solution should not be used more often, at higher doses than recommended, or in conjunction with other medications containing long-acting beta 2-agonists.
^4 Contraindications
Arformoterol Tartrate Inhalation Solution is contraindicated in patients with a history of hypersensitivity to arformoterol, racemic formoterol or to any other components of this product.
Use of a LABA, including Arformoterol Tartrate Inhalation Solution, without an inhaled cortisteroid is contraindicated in patients with asthma [ see Warnings and Precautions ( 5) ]. Arformoterol Tartrate Inhalation Solution is not indicated for the treatment of asthma.
^ Maintenance Treatment Of Copd
Arformoterol Tartrate Inhalation Solution is indicated for the long-term, twice daily (morning and evening) maintenance treatment of bronchoconstriction in patients with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and emphysema. Arformoterol Tartrate Inhalation Solution is for use by nebulization only.
^ How Supplied/storage And Handling
Arformoterol Tartrate Inhalation Solution is supplied in a single strength (15 mcg of arformoterol, equivalent to 22 mcg of arformoterol tartrate) as 2 mL of a sterile solution in low-density polyethylene (LDPE) unit-dose vials overwrapped in foil. Arformoterol Tartrate Inhalation Solution is available in a shelf-carton containing 30 or 60 unit-dose vials.
NDC 73289-0072-1: Foil pouch of 1 unit-dose vial NDC 73289-0072-2: Foil pouch of 4 unit-dose vial NDC 73289-0072-3: carton of 30 individually pouched unit-dose vials NDC 73289-0072-4: carton of 60 unit-dose vials (15x4 unit-dose vial pouches).
^ Geriatric Use
Of the 873 patients who received Arformoterol Tartrate Inhalation Solution in two placebo-controlled clinical studies in adults with COPD, 391 (45%) were 65 years of age or older while 96 (11%) were 75 years of age or older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Among subjects age 65 years and older, 129 (33%) received Arformoterol Tartrate Inhalation Solution at the recommended dose of 15 mcg twice daily, while the remainder received higher doses. ECG alerts for ventricular ectopy in patients 65 to ≤75 years of age were comparable among patients receiving 15 mcg twice daily, 25 mcg twice daily, and placebo (3.9%, 5.2%, and 7.1%, respectively). A higher frequency (12.4%) was observed when Arformoterol Tartrate Inhalation Solution was dosed at 50 mcg once daily. The clinical significance of this finding is not known. Other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
^ Beta 2-agonist Adverse Reaction Profile
Adverse reactions to Arformoterol Tartrate Inhalation Solution are expected to be similar in nature to other beta 2-adrenergic receptor agonists including: angina, hypertension or hypotension, tachycardia, arrhythmias, nervousness, headache, tremor, dry mouth, palpitation, muscle cramps, nausea, dizziness, fatigue, malaise, hypokalemia, hyperglycemia, metabolic acidosis and insomnia.
^ Xanthine Derivatives, Steroids, Or Diuretics
Concomitant treatment with methylxanthine (aminophylline, theophylline), steroids, or diuretics may potentiate any hypokalemic effect of adrenergic agonists including Arformoterol Tartrate Inhalation Solution [ see Warnings and Precautions ( 5.7) ].
The concurrent use of intravenously or orally administered methylxanthines (e.g., aminophylline, theophylline) by patients receiving Arformoterol Tartrate Inhalation Solution has not been completely evaluated. In two combined 12-week, placebo-controlled trials that included Arformoterol Tartrate Inhalation Solution doses of 15 mcg twice daily, 25 mcg twice daily, and 50 mcg once daily, 54 of 873 Arformoterol Tartrate Inhalation Solution-treated subjects received concomitant theophylline at study entry. In a 12-month controlled trial that included a 50 mcg once daily Arformoterol Tartrate Inhalation Solution dose, 30 of the 528 Arformoterol Tartrate Inhalation Solution-treated subjects received concomitant theophylline at study entry. In these trials, heart rate and systolic blood pressure were approximately 2-3 bpm and 6-8 mm Hg higher, respectively, in subjects on concomitant theophylline compared with the overall population.
^9 Drug Abuse And Dependence
There were no reported cases of abuse or evidence of drug dependence with the use of Arformoterol Tartrate Inhalation Solution in the clinical trials.
^ Important Limitations Of Use
Arformoterol Tartrate Inhalation Solution is not indicated to treat acute deteriorations of chronic obstructive pulmonary disease [ see Warnings and Precautions ( 5.2) ].
Arformoterol Tartrate Inhalation Solution is not indicated to treat asthma. The safety and effectiveness of Arformoterol Tartrate Inhalation Solution in asthma have not been established.
^ Renal Impairment
The systemic exposure to arformoterol was similar to renally impaired patients compared with demographically matched healthy control subjects [ see Clinical Pharmacology ( 12.3) ].
^ Non-potassium Sparing Diuretics
The ECG changes and/or hypokalemia that may result from the administration of non-potassium sparing diuretics (such as loop or thiazide diuretics) can be acutely worsened by beta-agonists, especially when the recommended dose of the beta-agonist is exceeded. Although the clinical significance of these effects is not known, caution is advised in the co-administration of beta-agonists, including Arformoterol Tartrate Inhalation Solution, with non-potassium sparing diuretics.
^ Carcinogenesis, Mutagenesis, Impairment Of Fertility
Long-term studies were conducted in mice using oral administration and rats using inhalation administration to evaluate the carcinogenic potential of arformoterol.
In a 24-month carcinogenicity study in CD-1 mice, arformoterol caused a dose-related increase in the incidence of uterine and cervical endometrial stromal polyps and stromal cell sarcoma in female mice at oral doses of 1,000 mcg/kg and above (AUC exposure approximately 70 times adult exposure at the MRHDID).
In a 24-month carcinogenicity study in Sprague-Dawley rats, arformoterol caused a statistically significant increase in the incidence of thyroid gland c-cell adenoma and carcinoma in female rats at an inhalation dose of 200 mcg/kg (AUC exposure approximately 130 times adult exposure at the MRHDID). There were no tumor findings with an inhalation dose of 40 mcg/kg (AUC exposure approximately 55 times adult exposure at the MRHDID).
Arformoterol was not mutagenic or clastogenic in the following tests: mutagenicity tests in bacteria, chromosome aberration analyses in mammalian cells, and micronucleus test in mice.
Arformoterol had no effects on fertility and reproductive performance in rats at oral doses up to 10,000 mcg/kg (approximately 3,200 times the MRHDID in adults on a mcg/m 2basis).
^Package Label.principal Display Panel
^ Immediate Hypersensitivity Reactions
Immediate hypersensitivity reactions may occur after administration of Arformoterol Tartrate Inhalation Solution as demonstrated by cases of anaphylactic reaction, urticaria, angioedema, rash and bronchospasm.
^ Beta-blockers
Beta-adrenergic receptor antagonists (beta-blockers) and Arformoterol Tartrate Inhalation Solution may inhibit the effect of each other when administered concurrently. Beta-blockers not only block the therapeutic effects of beta-agonists, but may produce severe bronchospasm in COPD patients. Therefore, patients with COPD should not normally be treated with beta-blockers. However, under certain circumstances, e.g., as prophylaxis after myocardial infarction, there may be no acceptable alternatives to the use of beta-blockers in patients with COPD. In this setting, cardioselective beta-blockers could be considered, although they should be administered with caution.
^6 Adverse Reactions
Long-acting beta 2-adrenergic agonists, such as Arformoterol Tartrate , as monotherapy (without inhaled corticosteroids) for asthma increase the risk of asthma-related events. Arformoterol Tartrate Inhalation Solution is not indicated for the treatment of asthma [see Warnings and Precautions ( 5.1)].
^ Deterioration Of Disease And Acute Episodes
Arformoterol Tartrate Inhalation Solution should not be initiated in patients with acutely deteriorating COPD, which may be a life-threatening condition. The use of Arformoterol Tartrate Inhalation Solution in this setting is inappropriate.
Arformoterol Tartrate Inhalation Solution is not indicated for the treatment of acute episodes of bronchospasm, i.e., as rescue therapy and extra doses should not be used for that purpose. Acute symptoms should be treated with an inhaled short-acting beta 2-agonist.
When beginning Arformoterol Tartrate Inhalation Solution, patients who have been taking inhaled short-acting beta 2-agonists on a regular basis (e.g., four times a day) should be instructed to discontinue the regular use of these drugs and use them only for symptomatic relief of acute respiratory symptoms. When prescribing Arformoterol Tartrate Inhalation Solution, the healthcare provider should also prescribe an inhaled, short-acting beta 2-agonist and instruct the patient how it should be used. Increasing inhaled beta 2-agonist use is a signal of deteriorating disease for which prompt medical attention is indicated. COPD may deteriorate acutely over a period of hours or chronically over several days or longer. If Arformoterol Tartrate Inhalation Solution no longer controls the symptoms of bronchoconstriction, or the patient's inhaled, short-acting beta 2-agonist becomes less effective or the patient needs more inhalation of short-acting beta 2-agonist than usual, these may be markers of deterioration of disease. In this setting, a reevaluation of the patient and the COPD treatment regimen should be undertaken at once. Increasing the daily dosage of Arformoterol Tartrate Inhalation Solution beyond the recommended 15 mcg twice daily dose is not appropriate in this situation.
^2 Dosage And Administration
The recommended dose of Arformoterol Tartrate Inhalation Solution is one 15 mcg unit-dose vial administered twice daily (morning and evening) by nebulization. A total daily dose of greater than 30 mcg (15 mcg twice daily) is not recommended.
Arformoterol Tartrate Inhalation Solution should be administered by the orally inhaled route via a standard jet nebulizer connected to an air compressor (see the accompanying Patient Information ). Arformoterol Tartrate Inhalation Solution should not be swallowed. Arformoterol Tartrate Inhalation Solution should be stored refrigerated in foil pouches. After opening the pouch, unused unit-dose vials should be returned to, and stored in, the pouch. An opened unit-dose vial should be used right away.
If the recommended maintenance treatment regimen fails to provide the usual response, medical advice should be sought immediately, as this is often a sign of destabilization of COPD. Under these circumstances, the therapeutic regimen should be reevaluated and additional therapeutic options should be considered.
No dose adjustment is required for patients with renal or hepatic impairment. However, since the clearance of Arformoterol Tartrate Inhalation Solution is prolonged in patients with hepatic impairment, they should be monitored closely.
The drug compatibility (physical and chemical), efficacy, and safety of Arformoterol Tartrate Inhalation Solution when mixed with other drugs in a nebulizer have not been established.
The safety and efficacy of Arformoterol Tartrate Inhalation Solution have been established in clinical trials when administered using the PARI LC ®Plus nebulizer (with a face mask or mouthpiece) and the PARI DURA NEB ™3000 compressor. The safety and efficacy of Arformoterol Tartrate Inhalation Solution delivered from non-compressor based nebulizer systems have not been established.
^ Pharmacokinetics
The pharmacokinetics (PK) of arformoterol have been investigated in healthy subjects, elderly subjects, renally and hepatically impaired subjects, and COPD patients following the nebulization of the recommended therapeutic dose and doses up to 96 mcg.
^ Pharmacogenomics
Arformoterol is eliminated through the action of multiple drug metabolizing enzymes. Direct glucuronidation of arformoterol is mediated by several UGT enzymes and is the primary elimination route. O-Desmethylation is a secondary route catalyzed by the CYP enzymes CYP2D6 and CYP2C19. In otherwise healthy subjects with reduced CYP2D6 and/or UGT1A1 enzyme activity, there was no impact on systemic exposure to arformoterol compared to subjects with normal CYP2D6 and/or UGT1A1 enzyme activities.
^ Hypokalemia And Hyperglycemia
Beta-agonist medications may produce significant hypokalemia in some patients, possibly through intracellular shunting, which has the potential to produce adverse cardiovascular effects [ see Clinical Pharmacology ( 12.2) ]. The decrease in serum potassium is usually transient, not requiring supplementation. Beta-agonist medications may produce transient hyperglycemia in some patients.
Clinically significant and dose-related changes in serum potassium and blood glucose were infrequent during clinical trials with long-term administration of Arformoterol Tartrate Inhalation Solution at the recommended dose.
^ Mao Inhibitors, Tricyclic Antidepressants, Qtc Prolonging Drugs
Arformoterol Tartrate Inhalation Solution, as with other beta-agonists, should be administered with extreme caution to patients being treated with monoamine oxidase inhibitors, tricyclic antidepressants, or drugs known to prolong the QTc interval because of the effect of adrenergic agonists on the cardiovascular system may be potentiated by these agents. Drugs that are known to prolong the QTc interval have an increased risk of ventricular arrhythmias.
^ Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
^ Mechanism Of Action
Arformoterol, the (R,R)-enantiomer of formoterol, is a selective long-acting beta 2-adrenergic receptor agonist (beta 2-agonist) that has two-fold greater potency than racemic formoterol (which contains both the (S,S) and (R,R)-enantiomers). The (S,S)-enantiomer is about 1,000-fold less potent as a beta 2-agonist than the (R,R)-enantiomer. While it is recognized that beta 2-receptors are the predominant adrenergic receptors in bronchial smooth muscle and beta 1-receptors are the predominant receptors in the heart, data indicate that there are also beta 2-receptors in the human heart comprising 10% to 50% of the total beta-adrenergic receptors. The precise function of these receptors has not been established, but they raise the possibility that even highly selective beta 2-agonists may have cardiac effects.
The pharmacologic effects of beta 2-adrenoceptor agonist drugs, including arformoterol, are at least in part attributable to stimulation of intracellular adenyl cyclase, the enzyme that catalyzes the conversion of adenosine triphosphate (ATP) to cyclic-3′,5′-adenosine monophosphate (cyclic AMP). Increased intracellular cyclic AMP levels cause relaxation of bronchial smooth muscle and inhibition of release of mediators of immediate hypersensitivity from cells, especially from mast cells.
In vitro tests show that arformoterol is an inhibitor of the release of mast cell mediators, such as histamine and leukotrienes, from the human lung. Arformoterol also inhibits histamine-induced plasma albumin extravasation in anesthetized guinea pigs and inhibits allergen-induced eosinophil influx in dogs with airway hyper-responsiveness. The relevance of these in vitro and animal findings to humans is unknown.