^
Manufactured for: Breckenridge Pharmaceutical, Inc.,Boca Raton, FL 33487
Manufactured by: Laboratorios Dr. Esteve, S.A.,Martorelles (Barcelona), Spain
^ Angle-closure Glaucoma
The pupillary dilation that occurs following use of many antidepressant drugs including duloxetine may trigger an angle closure attack in a patient with anatomically narrow angles who does not have a patent iridectomy.
^ Use In Patients With Concomitant Illness
Clinical experience with Duloxetine Delayed-release Capsules in patients with concomitant systemic illnesses is limited. There is no information on the effect that alterations in gastric motility may have on the stability of Duloxetine Delayed-release Capsules' enteric coating. In extremely acidic conditions, Duloxetine Delayed-release Capsules, unprotected by the enteric coating, may undergo hydrolysis to form naphthol. Caution is advised in using Duloxetine Delayed-release Capsules in patients with conditions that may slow gastric emptying (e.g., some diabetics).
Duloxetine Delayed-release Capsules have not been systematically evaluated in patients with a recent history of myocardial infarction or unstable coronary artery disease. Patients with these diagnoses were generally excluded from clinical studies during the product's premarketing testing.
^ Cns Drugs
[See Warnings and Precautions (5.12)].
^ Abuse
In animal studies, duloxetine did not demonstrate barbiturate-like (depressant) abuse potential.
While Duloxetine Delayed-release Capsules have not been systematically studied in humans for its potential for abuse, there was no indication of drug-seeking behavior in the clinical trials. However, it is not possible to predict on the basis of premarketing experience the extent to which a CNS active drug will be misused, diverted, and/or abused once marketed. Consequently, physicians should carefully evaluate patients for a history of drug abuse and follow such patients closely, observing them for signs of misuse or abuse of Duloxetine Delayed-release Capsules (e.g., development of tolerance, incrementation of dose, drug-seeking behavior).
^ Generalized Anxiety Disorder
The efficacy of Duloxetine Delayed-release Capsules in the treatment of generalized anxiety disorder (GAD) was established in 1 fixed-dose randomized, double-blind, placebo-controlled trial and 2 flexible-dose randomized, double-blind, placebo-controlled trials in adult outpatients between 18 and 83 years of age meeting the DSM-IV criteria for GAD.
In 1 flexible-dose study and in the fixed-dose study, the starting dose was 60 mg once daily where down titration to 30 mg once daily was allowed for tolerability reasons before increasing it to 60 mg once daily. Fifteen percent of patients were down titrated. One flexible-dose study had a starting dose of 30 mg once daily for 1 week before increasing it to 60 mg once daily.
The 2 flexible-dose studies involved dose titration with Duloxetine Delayed-release Capsules doses ranging from 60 mg once daily to 120 mg once daily (N=168 and N=162) compared to placebo (N=159 and N=161) over a 10-week treatment period. The mean dose for completers at endpoint in the flexible-dose studies was 104.75 mg/day. The fixed-dose study evaluated Duloxetine Delayed-release Capsules doses of 60 mg once daily (N=168) and 120 mg once daily (N=170) compared to placebo (N=175) over a 9-week treatment period. While a 120 mg/day dose was shown to be effective, there is no evidence that doses greater than 60 mg/day confer additional benefit.
In all 3 studies, Duloxetine Delayed-release Capsules demonstrated superiority over placebo as measured by greater improvement in the Hamilton Anxiety Scale (HAM-A) total score (Studies 1-3 in Table 8) and by the Sheehan Disability Scale (SDS) global functional impairment score. The SDS is a composite measurement of the extent emotional symptoms disrupt patient functioning in 3 life domains: work/school, social life/leisure activities, and family life/home responsibilities.
In another study, 887 patients meeting DSM-IV-TR criteria for GAD received Duloxetine Delayed-release Capsules 60 mg to 120 mg once daily during an initial 26-week open-label treatment phase. Four hundred and twenty-nine patients who responded to open-label treatment (defined as meeting the following criteria at weeks 24 and 26: a decrease from baseline HAM-A total score by at least 50% to a score no higher than 11, and a Clinical Global Impressions of Improvement [CGI-Improvement] score of 1 or 2) were randomly assigned to continuation of Duloxetine Delayed-release Capsules at the same dose (N=216) or to placebo (N=213) and were observed for relapse. Of the patients randomized, 73% had been in a responder status for at least 10 weeks. Relapse was defined as an increase in CGI-Severity score at least 2 points to a score ≥4 and a MINI (Mini-International Neuropsychiatric Interview) diagnosis of GAD (excluding duration), or discontinuation due to lack of efficacy. Patients taking Duloxetine Delayed-release Capsules experienced a statistically significantly longer time to relapse of GAD than did patients taking placebo (Study 4 in Figure 2).
Subgroup analyses did not indicate that there were any differences in treatment outcomes as a function of age or gender.
Pediatric use information for patients ages 7 to 17 years is approved for Eli Lilly and Company, Inc.'s CYMBALTA® (duloxetine) delayed-release capsules. However, due to Eli Lilly and Company, Inc.'s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
^ Adverse Reactions Occurring At An Incidence Of 5% Or More Among Duloxetine-treated Patients In Adult Placebo-controlled Trials
Table 2 gives the incidence of treatment-emergent adverse reactions in placebo-controlled trials for approved indications that occurred in 5% or more of patients treated with duloxetine and with an incidence greater than placebo.
^ Vital Sign Changes In Adults
In placebo-controlled clinical trials across approved indications for change from baseline to endpoint, duloxetine treatment was associated with mean increases of 0.23 mm Hg in systolic blood pressure and 0.73 mm Hg in diastolic blood pressure compared to mean decreases of 1.09 mm Hg systolic and 0.55 mm Hg diastolic in placebo-treated patients. There was no significant difference in the frequency of sustained (3 consecutive visits) elevated blood pressure [see Warnings and Precautions (5.3, 5.11)].
Duloxetine treatment, for up to 26 weeks in placebo-controlled trials across approved indications, typically caused a small increase in heart rate for change from baseline to endpoint compared to placebo of up to 1.37 beats per minute (increase of 1.20 beats per minute in duloxetine-treated patients, decrease of 0.17 beats per minute in placebo-treated patients).
^ Inhibitors Of Cyp2d6
Concomitant use of duloxetine (40 mg once daily) with paroxetine (20 mg once daily) increased the concentration of duloxetine AUC by about 60%, and greater degrees of inhibition are expected with higher doses of paroxetine. Similar effects would be expected with other potent CYP2D6 inhibitors (e.g., fluoxetine, quinidine) [see Warnings and Precautions (5.12)].
^ Chronic Musculoskeletal Pain
Duloxetine Delayed-release Capsules are indicated for the management of chronic musculoskeletal pain. This has been established in studies in patients with chronic low back pain and chronic pain due to osteoarthritis.
^Warning: Suicidal Thoughts And Behaviors
Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term studies. These studies did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in patients over age 24; there was a reduction in risk with antidepressant use in patients aged 65 and older [see Warnings and Precautions (5.1)].
In patients of all ages who are started on antidepressant therapy, monitor closely for worsening, and for emergence of suicidal thoughts and behaviors. Advise families and caregivers of the need for close observation and communication with the prescriber [see Warnings and Precautions (5.1)].
^ Abnormal Bleeding
SSRIs and SNRIs, including duloxetine, may increase the risk of bleeding events. Concomitant use of aspirin, nonsteroidal anti-inflammatory drugs, warfarin, and other anti-coagulants may add to this risk. Case reports and epidemiological studies (case-control and cohort design) have demonstrated an association between use of drugs that interfere with serotonin reuptake and the occurrence of gastrointestinal bleeding. Bleeding events related to SSRIs and SNRIs use have ranged from ecchymoses, hematomas, epistaxis, and petechiae to life-threatening hemorrhages.
Patients should be cautioned about the risk of bleeding associated with the concomitant use of duloxetine and NSAIDs, aspirin, or other drugs that affect coagulation.
^ Clinical Trial Data Sources
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The stated frequencies of adverse reactions represent the proportion of individuals who experienced, at least once, a treatment-emergent adverse reaction of the type listed. A reaction was considered treatment-emergent if it occurred for the first time or worsened while receiving therapy following baseline evaluation. Reactions reported during the studies were not necessarily caused by the therapy, and the frequencies do not reflect investigator impression (assessment) of causality.
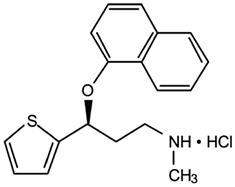
^ . Description
Duloxetine Delayed-release Capsules (duloxetine hydrochloride) are a selective serotonin and norepinephrine reuptake inhibitor (SSNRI) for oral administration. Its chemical designation is (+)-(S)-N-methyl-γ-(1-naphthyloxy)-2-thiophenepropylamine hydrochloride. The empirical formula is C18H19NOS∙HCl, which corresponds to a molecular weight of 333.88. The structural formula is:
Duloxetine hydrochloride is a white to slightly brownish white solid, which is slightly soluble in water.
Each capsule contains enteric-coated pellets of 22.4, 33.7, or 67.3 mg of duloxetine hydrochloride equivalent to 20, 30, or 60 mg of duloxetine, respectively. These enteric-coated pellets are designed to prevent degradation of the drug in the acidic environment of the stomach. Inactive ingredients include ammonium hydroxide, black iron oxide, hypromellose, methacrylic acid copolymer dispersion (methacrylic acid-ethyl acrylate copolymer, polysorbate 80, sodium lauryl sulfate), potassium hydroxide, propylene glycol, shellac, sucrose, sugar spheres (maize starch, sucrose), talc, titanium dioxide, triethylcitrate, and hard gelatin capsules (gelatin, titanium dioxide). The 20 mg hard gelatin capsule colorant is yellow iron oxide. The 30 mg hard gelatin capsule colorants are FD&C Blue No. 1, FD&C Yellow No. 6, and FD&C Yellow No. 10. The 60 mg hard gelatin capsule colorants are FD&C Blue No. 1, FD&C Yellow No. 6, FD&C Yellow No.10, and yellow iron oxide.
^ Urinary Hesitation And Retention
Duloxetine Delayed-release Capsules are in a class of drugs known to affect urethral resistance. If symptoms of urinary hesitation develop during treatment with Duloxetine Delayed-release Capsules, consideration should be given to the possibility that they might be drug-related.
In post marketing experience, cases of urinary retention have been observed. In some instances of urinary retention associated with duloxetine use, hospitalization and/or catheterization has been needed.
^ Drugs That Affect Gastric Acidity
Duloxetine Delayed-release Capsules have an enteric coating that resists dissolution until reaching a segment of the gastrointestinal tract where the pH exceeds 5.5. In extremely acidic conditions, Duloxetine Delayed-release Capsules, unprotected by the enteric coating, may undergo hydrolysis to form naphthol. Caution is advised in using Duloxetine Delayed-release Capsules in patients with conditions that may slow gastric emptying (e.g., some diabetics). Drugs that raise the gastrointestinal pH may lead to an earlier release of duloxetine. However, co-administration of Duloxetine Delayed-release Capsules with aluminum- and magnesium-containing antacids (51 mEq) or Duloxetine Delayed-release Capsules with famotidine, had no significant effect on the rate or extent of duloxetine absorption after administration of a 40 mg oral dose. It is unknown whether the concomitant administration of proton pump inhibitors affects duloxetine absorption [see Warnings and Precautions (5.14)].
^ Dosage For Treatment Of Chronic Musculoskeletal Pain
Administer Duloxetine Delayed-release Capsules 60 mg once daily. Begin treatment at 30 mg for one week, to allow patients to adjust to the medication before increasing to 60 mg once daily. There is no evidence that higher doses confer additional benefit, even in patients who do not respond to a 60 mg dose, and higher doses are associated with a higher rate of adverse reactions [see Clinical Studies (14.5)].
^4. Contraindications
Monoamine Oxidase Inhibitors (MAOIs) — The use of MAOIs intended to treat psychiatric disorders with Duloxetine Delayed-release Capsules or within 5 days of stopping treatment with Duloxetine Delayed-release Capsules is contraindicated because of an increased risk of serotonin syndrome. The use of Duloxetine Delayed-release Capsules within 14 days of stopping an MAOI intended to treat psychiatric disorders is also contraindicated [see Dosage and Administration (2.8) and Warnings and Precautions (5.4)].
Starting Duloxetine Delayed-release Capsules in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue is also contraindicated because of an increased risk of serotonin syndrome [see Dosage and Administration (2.9) and Warnings and Precautions (5.4)].
^ Electrocardiogram Changes In Adults
The effect of duloxetine 160 mg and 200 mg administered twice daily to steady state was evaluated in a randomized, double-blinded, two-way crossover study in 117 healthy female subjects. No QT interval prolongation was detected. Duloxetine appears to be associated with concentration-dependent but not clinically meaningful QT shortening.
^ Drugs Metabolized By Cyp2d6
Duloxetine is a moderate inhibitor of CYP2D6. When duloxetine was administered (at a dose of 60 mg twice daily) in conjunction with a single 50 mg dose of desipramine, a CYP2D6 substrate, the AUC of desipramine increased 3-fold [see Warnings and Precautions (5.12)].
^ Adverse Reactions Observed In Children And Adolescent Placebo-controlled Clinical Trials
The adverse drug reaction profile observed in pediatric clinical trials (children and adolescents) was consistent with the adverse drug reaction profile observed in adult clinical trials. The specific adverse drug reactions observed in adult patients can be expected to be observed in pediatric patients (children and adolescents) [see Adverse Reactions (6.5)]. The most common (≥5% and twice placebo) adverse reactions observed in pediatric clinical trials include: nausea, diarrhea, decreased weight, and dizziness.
Table 6 provides the incidence of treatment-emergent adverse reactions in pediatric placebo-controlled trials that occurred in greater than 2% of patients treated with Duloxetine Delayed-release Capsules and with an incidence greater than placebo.
Other adverse reactions that occurred at an incidence of less than 2% but were reported by more duloxetine treated patients than placebo treated patients and are associated Duloxetine Delayed-release Capsules treatment: abnormal dreams (including nightmare), anxiety, flushing (including hot flush), hyperhidrosis, palpitations, pulse increased, and tremor.
Discontinuation-emergent symptoms have been reported when stopping Duloxetine Delayed-release Capsules. The most commonly reported symptoms following discontinuation of Duloxetine Delayed-release Capsules in pediatric clinical trials have included headache, dizziness, insomnia, and abdominal pain [see Warnings and Precautions (5.7) and Adverse Reactions (6.2)].
^Medication Guide
Duloxetine (doo-LOX-e-teen)
Delayed-release Capsules, USP
Rx Only
Read this Medication Guide before you start taking Duloxetine Delayed-release Capsules and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment.
Talk to your healthcare provider about:
What is the most important information I should know about antidepressant medicines, depression, other serious mental illnesses, and suicidal thoughts or actions?
Call your healthcare provider right away if you have any of the following symptoms or feelings, especially if they are new, worse, or worry you. In an emergency, call 911.
What else do I need to know about antidepressant medicines?
What are Duloxetine Delayed-release Capsules?
Duloxetine Delayed-release Capsules are a prescription medicine used to treat a certain type of depression called Major Depressive Disorder (MDD). Duloxetine Delayed-release Capsules belong to a class of medicines known as SNRIs (or serotonin-norepinephrine reuptake inhibitors).
Duloxetine Delayed-release Capsules are also used to treat or manage:
Who should not take Duloxetine Delayed-release Capsules?
Do Not take Duloxetine Delayed-release Capsules if you:
People who take Duloxetine Delayed-release Capsules close in time to an MAOI may have a serious problem called Serotonin Syndrome (see "What are the possible side effects of Duloxetine Delayed-release Capsules?").
What should I tell my healthcare provider before taking Duloxetine Delayed-release Capsules?
Before starting Duloxetine Delayed-release Capsules, tell your healthcare provider if you:
Tell your healthcare provider about all the medicines that you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Duloxetine Delayed-release Capsules and some medicines may interact with each other, may not work as well, or may cause serious side effects.
Especially tell your healthcare provider if you take:
Ask your healthcare provider for a list of these medicines if you are not sure.
Do not take Duloxetine Delayed-release Capsules with any other medicine that contain duloxetine.
How should I take Duloxetine Delayed-release Capsules?
What should I avoid while taking Duloxetine Delayed-release Capsules?
What are the possible side effects of Duloxetine Delayed-release Capsules?
Duloxetine Delayed-release Capsules may cause serious side effects, including: See "What is the most important information I should know about Duloxetine Delayed-release Capsules?"
Common possible side effects in people who take Duloxetine Delayed-release Capsules include:
The most common side effects of Duloxetine Delayed-release Capsules include:
Common possible side effects in children and adolescents who take Duloxetine Delayed-release Capsules include:
Side effects in adults may also occur in children and adolescents who take Duloxetine Delayed-release Capsules. Children and adolescents should have height and weight monitored during treatment.
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of Duloxetine Delayed-release Capsules. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to 1-800-FDA-1088.
How should I store Duloxetine Delayed-release Capsules?
Store Duloxetine Delayed-release Capsules at room temperature between 68°F to 77°F (20°C to 25°C).
Keep Duloxetine Delayed-release Capsules and all medicines out of the reach of children.
General information about the safe and effective use of Duloxetine Delayed-release Capsules.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use Duloxetine Delayed-release Capsules for a condition for which it was not prescribed. Do not give Duloxetine Delayed-release Capsules to other people, even if they have the same symptoms that you have. It may harm them.
This Medication Guide summarizes the most important information about Duloxetine Delayed-release Capsules. If you would like more information, talk with your healthcare provider. You may ask your healthcare provider or pharmacist for information about Duloxetine Delayed-release Capsules that is written for healthcare professionals.
For more information about Duloxetine Delayed-release Capsules contact Breckenridge Pharmaceutical, Inc. at 1-800-367-3395.
What are the ingredients in Duloxetine Delayed-release Capsules, USP?
Active ingredient: duloxetine hydrochloride, USP
Inactive ingredients: ammonium hydroxide, black iron oxide, hypromellose, methacrylic acid copolymer dispersion (methacrylic acid-ethyl acrylate copolymer, polysorbate 80, sodium lauryl sulfate), potassium hydroxide, propylene glycol, shellac, sucrose, sugar spheres (maize starch, sucrose), talc, titanium dioxide, triethylcitrate, and hard gelatin capsules (gelatin, titanium dioxide). The 20 mg hard gelatin capsule colorant is yellow iron oxide. The 30 mg hard gelatin capsule colorants are FD&C Blue No. 1, FD&C Yellow No. 6, and FD&C Yellow No. 10. The 60 mg hard gelatin capsule colorants are FD&C Blue No. 1, FD&C Yellow No. 6, FD&C Yellow No.10, and yellow iron oxide.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Trademarks are the property of their respective owners.
Revised: 02/2016
Manufactured for: Breckenridge Pharmaceutical, Inc.,Boca Raton, FL 33487
Manufactured by: Laboratorios Dr. Esteve, S.A.,Martorelles (Barcelona), Spain
^3. Dosage Forms And Strengths
Duloxetine Delayed-release Capsules are available as:
20 mg opaque ochre capsules imprinted with "B" on the cap and "746" on the body.
30 mg opaque green (cap) /opaque white (body) capsules imprinted with "B" on the cap and "747" on the body.
60 mg opaque green (cap) /opaque ochre (body) capsules imprinted with "B" on the cap and "748" on the body.
^ Signs And Symptoms
In postmarketing experience, fatal outcomes have been reported for acute overdoses, primarily with mixed overdoses, but also with duloxetine only, at doses as low as 1000 mg. Signs and symptoms of overdose (duloxetine alone or with mixed drugs) included somnolence, coma, serotonin syndrome, seizures, syncope, tachycardia, hypotension, hypertension, and vomiting.
^ Severe Skin Reactions
Severe skin reactions, including erythema multiforme and Stevens-Johnson Syndrome (SJS), can occur with Duloxetine Delayed-release Capsules. The reporting rate of SJS associated with Duloxetine Delayed-release Capsules use exceeds the general population background incidence rate for this serious skin reaction (1 to 2 cases per million person years). The reporting rate is generally accepted to be an underestimate due to underreporting.
Duloxetine Delayed-release Capsules should be discontinued at the first appearance of blisters, peeling rash, mucosal erosions, or any other sign of hypersensitivity if no other etiology can be identified.
^ Inhibitors Of Cyp1a2
When duloxetine 60 mg was co-administered with fluvoxamine 100 mg, a potent CYP1A2 inhibitor, to male subjects (n=14) duloxetine AUC was increased approximately 6-fold, the Cmax was increased about 2.5-fold, and duloxetine t1/2 was increased approximately 3-fold. Other drugs that inhibit CYP1A2 metabolism include cimetidine and quinolone antimicrobials such as ciprofloxacin and enoxacin [see Warnings and Precautions (5.12)].
^ Hepatotoxicity
There have been reports of hepatic failure, sometimes fatal, in patients treated with Duloxetine Delayed-release Capsules. These cases have presented as hepatitis with abdominal pain, hepatomegaly, and elevation of transaminase levels to more than twenty times the upper limit of normal with or without jaundice, reflecting a mixed or hepatocellular pattern of liver injury. Duloxetine Delayed-release Capsules should be discontinued in patients who develop jaundice or other evidence of clinically significant liver dysfunction and should not be resumed unless another cause can be established.
Cases of cholestatic jaundice with minimal elevation of transaminase levels have also been reported. Other postmarketing reports indicate that elevated transaminases, bilirubin, and alkaline phosphatase have occurred in patients with chronic liver disease or cirrhosis.
Duloxetine Delayed-release Capsules increased the risk of elevation of serum transaminase levels in development program clinical trials. Liver transaminase elevations resulted in the discontinuation of 0.3% (92/34,756) of Duloxetine Delayed-release Capsules-treated patients. In most patients, the median time to detection of the transaminase elevation was about two months. In adult placebo-controlled trials in any indication, for patients with normal and abnormal baseline ALT values, elevation of ALT >3 times the upper limit of normal occurred in 1.25% (144/11,496) of Duloxetine Delayed-release Capsules-treated patients compared to 0.45% (39/8716) of placebo-treated patients. In adult placebo-controlled studies using a fixed dose design, there was evidence of a dose response relationship for ALT and AST elevation of >3 times the upper limit of normal and >5 times the upper limit of normal, respectively.
Because it is possible that duloxetine and alcohol may interact to cause liver injury or that duloxetine may aggravate pre-existing liver disease, Duloxetine Delayed-release Capsules should not be prescribed to patients with substantial alcohol use or evidence of chronic liver disease.
^ Drugs Metabolized By Cyp1a2
In vitro drug interaction studies demonstrate that duloxetine does not induce CYP1A2 activity. Therefore, an increase in the metabolism of CYP1A2 substrates (e.g., theophylline, caffeine) resulting from induction is not anticipated, although clinical studies of induction have not been performed. Duloxetine is an inhibitor of the CYP1A2 isoform in in vitro studies, and in two clinical studies the average (90% confidence interval) increase in theophylline AUC was 7% (1%-15%) and 20% (13%-27%) when co-administered with duloxetine (60 mg twice daily).
^ Pharmacodynamics
Preclinical studies have shown that duloxetine is a potent inhibitor of neuronal serotonin and norepinephrine reuptake and a less potent inhibitor of dopamine reuptake. Duloxetine has no significant affinity for dopaminergic, adrenergic, cholinergic, histaminergic, opioid, glutamate, and GABA receptors in vitro. Duloxetine does not inhibit monoamine oxidase (MAO).
Duloxetine Delayed-release Capsules is in a class of drugs known to affect urethral resistance. If symptoms of urinary hesitation develop during treatment with Duloxetine Delayed-release Capsules, consideration should be given to the possibility that they might be drug-related.
^ Activation Of Mania/hypomania
In adult placebo-controlled trials in patients with major depressive disorder, activation of mania or hypomania was reported in 0.1% (4/3779) of duloxetine-treated patients and 0.04% (1/2536) of placebo-treated patients. No activation of mania or hypomania was reported in DPNP, GAD, or chronic musculoskeletal pain placebo-controlled trials. Activation of mania or hypomania has been reported in a small proportion of patients with mood disorders who were treated with other marketed drugs effective in the treatment of major depressive disorder. As with these other agents, Duloxetine Delayed-release Capsules should be used cautiously in patients with a history of mania.
^ Clinically Important Drug Interactions
Both CYP1A2 and CYP2D6 are responsible for duloxetine metabolism.
^ Laboratory Tests
No specific laboratory tests are recommended.
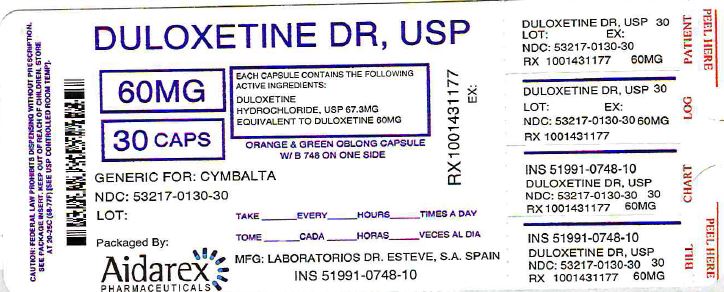
^ . How Supplied/storage And Handling
Duloxetine Delayed-release Capsules are available as delayed release capsules as Opaque Ochre, Opaque Green capsules, with 'B' on one side and "748" on the other.
90 CAPSULE in a BOTTLE (53217-130-90)
30 CAPSULE in a BOTTLE (53217-130-30)
60 CAPSULE in a BOTTLE (53217-130-60)
Store at 25°C (77°F); excursions permitted to 15-30°C (59-86°F) [see USP Controlled Room Temperature].
Repackaged by
Aidarex Pharmaceuticals, LLC
Corona, CA 92880
^ Switching A Patient To Or From A Monoamine Oxidase Inhibitor (maoi) Intended To Treat Psychiatric Disorders
At least 14 days should elapse between discontinuation of an MAOI intended to treat psychiatric disorders and initiation of therapy with Duloxetine Delayed-release Capsules. Conversely, at least 5 days should be allowed after stopping Duloxetine Delayed-release Capsules before starting an MAOI intended to treat psychiatric disorders [see Contraindications (4)].
^ Temazepam
Under steady-state conditions for duloxetine (20 mg qhs) and temazepam (30 mg qhs), the pharmacokinetics of duloxetine were not affected by co-administration.
^ Hepatic Impairment
Patients with clinically evident hepatic impairment have decreased duloxetine metabolism and elimination. After a single 20 mg dose of Duloxetine Delayed-release Capsules, 6 cirrhotic patients with moderate liver impairment (Child-Pugh Class B) had a mean plasma duloxetine clearance about 15% that of age- and gender-matched healthy subjects, with a 5-fold increase in mean exposure (AUC). Although Cmax was similar to normals in the cirrhotic patients, the half-life was about 3 times longer [see Dosage and Administration (2.6) and Warnings and Precautions (5.14)].
^ . Clinical Studies
The efficacy of duloxetine has been established in the following adequate and well-controlled trials:
Pediatric use information for patients ages 7 to 17 years is approved for Eli Lilly and Company, Inc.'s CYMBALTA® (duloxetine) delayed-release capsules. However, due to Eli Lilly and Company, Inc.'s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
^7. Drug Interactions
Both CYP1A2 and CYP2D6 are responsible for duloxetine metabolism.
^ Monoamine Oxidase Inhibitors (maois)
[See Dosage and Administration (2.8, 2.9), Contraindications (4), and Warnings and Precautions (5.4)].
^Principal Display Panel - Mg Capsule Bottle Label
^ Seizures
Duloxetine has not been systematically evaluated in patients with a seizure disorder, and such patients were excluded from clinical studies. In adult placebo-controlled clinical trials, seizures/convulsions occurred in 0.02% (3/12,722) of patients treated with duloxetine and 0.01% (1/9513) of patients treated with placebo. Duloxetine Delayed-release Capsules should be prescribed with care in patients with a history of a seizure disorder.
^ Alcohol
When Duloxetine Delayed-release Capsules and ethanol were administered several hours apart so that peak concentrations of each would coincide, Duloxetine Delayed-release Capsules did not increase the impairment of mental and motor skills caused by alcohol.
In the Duloxetine Delayed-release Capsules clinical trials database, three Duloxetine Delayed-release Capsules-treated patients had liver injury as manifested by ALT and total bilirubin elevations, with evidence of obstruction. Substantial intercurrent ethanol use was present in each of these cases, and this may have contributed to the abnormalities seen [see Warnings and Precautions (5.2, 5.12)].
^2. Dosage And Administration
Swallow Duloxetine Delayed-release Capsules whole. Do not chew or crush. Do not open the capsule and sprinkle its contents on food or mix with liquids. All of these might affect the enteric coating. Duloxetine Delayed-release Capsules can be given without regard to meals. If a dose of Duloxetine Delayed-release Capsules is missed, take the missed dose as soon as it is remembered. If it is almost time for the next dose, skip the missed dose and take the next dose at the regular time. Do not take two doses of Duloxetine Delayed-release Capsules at the same time.
^ Dual Inhibition Of Cyp1a2 And Cyp2d6
Concomitant administration of duloxetine 40 mg twice daily with fluvoxamine 100 mg, a potent CYP1A2 inhibitor, to CYP2D6 poor metabolizer subjects (n=14) resulted in a 6-fold increase in duloxetine AUC and Cmax.
^ Dependence
In drug dependence studies, duloxetine did not demonstrate dependence-producing potential in rats.
^ Discontinuing Duloxetine Delayed-release Capsules
Adverse reactions after discontinuation of Duloxetine Delayed-release Capsules, after abrupt or tapered discontinuation, include: dizziness, headache, nausea, diarrhea, paresthesia, irritability, vomiting, insomnia, anxiety, hyperhidrosis, and fatigue. A gradual reduction in dosage rather than abrupt cessation is recommended whenever possible [see Warnings and Precautions (5.7)].
^ Drugs Metabolized By Cyp2c
Results of in vitro studies demonstrate that duloxetine does not inhibit CYP2C19 activity at therapeutic concentrations. Inhibition of the metabolism of CYP2C19 substrates is therefore not anticipated, although clinical studies have not been performed.
^ . Patient Counseling Information
See FDA-approved patient labeling (Medication Guide).
^ Pediatric Use
The safety and effectiveness in pediatric patients less than 7 years of age have not been established.
Safety and effectiveness of Duloxetine Delayed-release Capsules have not been established in pediatric patients less than 18 years of age with MDD.
Decreased appetite and weight loss have been observed in association with the use of SSRIs and SNRIs. Perform regular monitoring of weight and growth in children and adolescents treated with an SNRI such as duloxetine [see Adverse Reactions (6.11)].
Information describing two additional clinical studies in which efficacy was not demonstrated in patients ages 7 to 17 years is approved for Eli Lilly and Company, Inc.'s CYMBALTA® (duloxetine) delayed-release capsules. Other pediatric use information for patients ages 7 to 17 years is approved for Eli Lilly and Company, Inc.'s CYMBALTA® (duloxetine) delayed-release capsules. However, due to Eli Lilly and Company, Inc.'s marketing exclusivity rights, this drug product is not labeled with that pediatric information.
^ Laboratory Changes In Adults
Duloxetine Delayed-release Capsule treatment in placebo-controlled clinical trials across approved indications, was associated with small mean increases from baseline to endpoint in ALT, AST, CPK, and alkaline phosphatase; infrequent, modest, transient, abnormal values were observed for these analytes in Duloxetine Delayed-release Capsules-treated patients when compared with placebo-treated patients [see Warnings and Precautions (5.2)]. High bicarbonate, cholesterol, and abnormal (high or low) potassium, were observed more frequently in Duloxetine Delayed-release Capsules treated patients compared to placebo.
^ Serotonergic Drugs
[See Dosage and Administration (2.8, 2.9), Contraindications (4), and Warnings and Precautions (5.4)].
^6. Adverse Reactions
The following serious adverse reactions are described below and elsewhere in the labeling:
^ Postmarketing Spontaneous Reports
The following adverse reactions have been identified during post approval use of Duloxetine Delayed-release Capsules. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Adverse reactions reported since market introduction that were temporally related to duloxetine therapy and not mentioned elsewhere in labeling include: anaphylactic reaction, aggression and anger (particularly early in treatment or after treatment discontinuation), angioneurotic edema, angle-closure glaucoma, extrapyramidal disorder, galactorrhea, gynecological bleeding, hallucinations, hyperglycemia, hyperprolactinemia, hypersensitivity, hypertensive crisis, muscle spasm, rash, restless legs syndrome, seizures upon treatment discontinuation, supraventricular arrhythmia, tinnitus (upon treatment discontinuation), trismus, and urticaria.
^ Major Depressive Disorder
The efficacy of Duloxetine Delayed-release Capsules as a treatment for depression was established in 4 randomized, double-blind, placebo-controlled, fixed-dose studies in adult outpatients (18 to 83 years) meeting DSM-IV criteria for major depression. In 2 studies, patients were randomized to Duloxetine Delayed-release Capsules 60 mg once daily (N=123 and N=128, respectively) or placebo (N=122 and N=139, respectively) for 9 weeks; in the third study, patients were randomized to Duloxetine Delayed-release Capsules 20 or 40 mg twice daily (N=86 and N=91, respectively) or placebo (N=89) for 8 weeks; in the fourth study, patients were randomized to Duloxetine Delayed-release Capsules 40 or 60 mg twice daily (N=95 and N=93, respectively) or placebo (N=93) for 8 weeks. There is no evidence that doses greater than 60 mg/day confer additional benefits.
In all 4 studies, Duloxetine Delayed-release Capsules demonstrated superiority over placebo as measured by improvement in the 17-item Hamilton Depression Rating Scale (HAMD-17) total score (Studies 1-4 in Table 7).
In all of these clinical studies, analyses of the relationship between treatment outcome and age, gender, and race did not suggest any differential responsiveness on the basis of these patient characteristics.
In another study, 533 patients meeting DSM-IV criteria for MDD received Duloxetine Delayed-release Capsules 60 mg once daily during an initial 12-week open-label treatment phase. Two hundred and seventy-eight patients who responded to open label treatment (defined as meeting the following criteria at weeks 10 and 12: a HAMD-17 total score ≤9, Clinical Global Impressions of Severity (CGI-S) ≤2, and not meeting the DSM-IV criteria for MDD) were randomly assigned to continuation of Duloxetine Delayed-release Capsules at the same dose (N=136) or to placebo (N=142) for 6 months. Patients on Duloxetine Delayed-release Capsules experienced a statistically significantly longer time to relapse of depression than did patients on placebo (Study 5 in Figure 1). Relapse was defined as an increase in the CGI-S score of ≥2 points compared with that obtained at week 12, as well as meeting the DSM-IV criteria for MDD at 2 consecutive visits at least 2 weeks apart, where the 2-week temporal criterion had to be satisfied at only the second visit. The effectiveness of Duloxetine Delayed-release Capsules in hospitalized patients with major depressive disorder has not been studied.
^ Effect On Blood Pressure
In adult placebo-controlled clinical trials across indications from baseline to endpoint, duloxetine treatment was associated with mean increases of 0.5 mm Hg in systolic blood pressure and 0.8 mm Hg in diastolic blood pressure compared to mean decreases of 0.6 mm Hg systolic and 0.3 mm Hg diastolic in placebo-treated patients. There was no significant difference in the frequency of sustained (3 consecutive visits) elevated blood pressure. In a clinical pharmacology study designed to evaluate the effects of duloxetine on various parameters, including blood pressure at supratherapeutic doses with an accelerated dose titration, there was evidence of increases in supine blood pressure at doses up to 200 mg twice daily. At the highest 200 mg twice daily dose, the increase in mean pulse rate was 5.0 to 6.8 beats and increases in mean blood pressure were 4.7 to 6.8 mm Hg (systolic) and 4.5 to 7 mm Hg (diastolic) up to 12 hours after dosing.
Blood pressure should be measured prior to initiating treatment and periodically measured throughout treatment [see Adverse Reactions (6.7)].
^1. Indications And Usage
Duloxetine Delayed-release Capsules are indicated for the treatment of:
^ Orthostatic Hypotension, Falls And Syncope
Orthostatic hypotension, falls and syncope have been reported with therapeutic doses of duloxetine. Syncope and orthostatic hypotension tend to occur within the first week of therapy but can occur at any time during duloxetine treatment, particularly after dose increases. The risk of falling appears to be related to the degree of orthostatic decrease in blood pressure as well as other factors that may increase the underlying risk of falls.
In an analysis of patients from all placebo-controlled trials, patients treated with duloxetine reported a higher rate of falls compared to patients treated with placebo. Risk appears to be related to the presence of orthostatic decrease in blood pressure. The risk of blood pressure decreases may be greater in patients taking concomitant medications that induce orthostatic hypotension (such as antihypertensives) or are potent CYP1A2 inhibitors [see Warnings and Precautions (5.12) and Drug Interactions (7.1)] and in patients taking duloxetine at doses above 60 mg daily. Consideration should be given to dose reduction or discontinuation of Duloxetine Delayed-release Capsules in patients who experience symptomatic orthostatic hypotension, falls and/or syncope during duloxetine therapy.
Risk of falling also appeared to be proportional to a patient's underlying risk for falls and appeared to increase steadily with age. As elderly patients tend to have a higher underlying risk for falls due to a higher prevalence of risk factors such as use of multiple medications, medical comorbidities and gait disturbances, the impact of increasing age by itself is unclear. Falls with serious consequences including bone fractures and hospitalizations have been reported [see Adverse Reactions (6.10) and Patient Counseling Information (17)].
^ Geriatric Use
Of the 2,418 patients in premarketing clinical studies of Duloxetine Delayed-release Capsules for MDD, 5.9% (143) were 65 years of age or over. Of the 1041 patients in CLBP premarketing studies, 21.2% (221) were 65 years of age or over. Of the 487 patients in OA premarketing studies, 40.5% (197) were 65 years of age or over. Of the 1,074 patients in the DPNP premarketing studies, 33% (357) were 65 years of age or over. In the MDD, DPNP, OA, CLBP and other studies, no overall differences in safety or effectiveness were generally observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out. SSRIs and SNRIs, including Duloxetine Delayed-release Capsules have been associated with cases of clinically significant hyponatremia in elderly patients, who may be at greater risk for this adverse event [see Warnings and Precautions (5.13)].
In an analysis of data from all placebo-controlled-trials, patients treated with Duloxetine Delayed-release Capsules reported a higher rate of falls compared to patients treated with placebo. The increased risk appears to be proportional to a patient's underlying risk for falls. Underlying risk appears to increase steadily with age. As elderly patients tend to have a higher prevalence of risk factors for falls such as medications, medical comorbidities and gait disturbances, the impact of increasing age by itself on falls during treatment with Duloxetine Delayed-release Capsules is unclear. Falls with serious consequences including bone fractures and hospitalizations have been reported [see Warnings and Precautions (5.3) and Adverse Reactions (6.10)].
^ Drugs Metabolized By Cyp3a
Results of in vitro studies demonstrate that duloxetine does not inhibit or induce CYP3A activity. Therefore, an increase or decrease in the metabolism of CYP3A substrates (e.g., oral contraceptives and other steroidal agents) resulting from induction or inhibition is not anticipated, although clinical studies have not been performed.
^ Hyponatremia
Hyponatremia may occur as a result of treatment with SSRIs and SNRIs, including Duloxetine Delayed-release Capsules. In many cases, this hyponatremia appears to be the result of the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Cases with serum sodium lower than 110 mmol/L have been reported and appeared to be reversible when Duloxetine Delayed-release Capsules were discontinued. Elderly patients may be at greater risk of developing hyponatremia with SSRIs and SNRIs. Also, patients taking diuretics or who are otherwise volume depleted may be at greater risk [see Use in Specific Populations (8.5)]. Discontinuation of Duloxetine Delayed-release Capsules should be considered in patients with symptomatic hyponatremia and appropriate medical intervention should be instituted.
Signs and symptoms of hyponatremia include headache, difficulty concentrating, memory impairment, confusion, weakness, and unsteadiness, which may lead to falls. More severe and/or acute cases have been associated with hallucination, syncope, seizure, coma, respiratory arrest, and death.
^ Dosage For Treatment Of Major Depressive Disorder
Administer Duloxetine Delayed-release Capsules at a total dose of 40 mg/day (given as 20 mg twice daily) to 60 mg/day (given either once daily or as 30 mg twice daily). For some patients, it may be desirable to start at 30 mg once daily for 1 week, to allow patients to adjust to the medication before increasing to 60 mg once daily. While a 120 mg/day dose was shown to be effective, there is no evidence that doses greater than 60 mg/day confer any additional benefits. The safety of doses above 120 mg/day has not been adequately evaluated. Periodically reassess to determine the need for maintenance treatment and the appropriate dose for such treatment [see Clinical Studies (14.1)].
^ Diabetic Peripheral Neuropathic Pain
The efficacy of Duloxetine Delayed-release Capsules for the management of neuropathic pain associated with diabetic peripheral neuropathy was established in 2 randomized, 12-week, double-blind, placebo-controlled, fixed-dose studies in adult patients having diabetic peripheral neuropathic pain for at least 6 months. Study DPNP-1 and Study DPNP-2 enrolled a total of 791 patients of whom 592 (75%) completed the studies. Patients enrolled had Type I or II diabetes mellitus with a diagnosis of painful distal symmetrical sensorimotor polyneuropathy for at least 6 months. The patients had a baseline pain score of ≥4 on an 11-point scale ranging from 0 (no pain) to 10 (worst possible pain). Patients were permitted up to 4 g of acetaminophen per day as needed for pain, in addition to Duloxetine Delayed-release Capsules. Patients recorded their pain daily in a diary.
Both studies compared Duloxetine Delayed-release Capsules 60 mg once daily or 60 mg twice daily with placebo. DPNP-1 additionally compared Duloxetine Delayed-release Capsules 20 mg with placebo. A total of 457 patients (342 Duloxetine Delayed-release Capsules, 115 placebo) were enrolled in DPNP-1 and a total of 334 patients (226 Duloxetine Delayed-release Capsules, 108 placebo) were enrolled in DPNP-2. Treatment with Duloxetine Delayed-release Capsules 60 mg one or two times a day statistically significantly improved the endpoint mean pain scores from baseline and increased the proportion of patients with at least a 50% reduction in pain scores from baseline. For various degrees of improvement in pain from baseline to study endpoint, Figures 3 and 4 show the fraction of patients achieving that degree of improvement. The figures are cumulative, so that patients whose change from baseline is, for example, 50%, are also included at every level of improvement below 50%. Patients who did not complete the study were assigned 0% improvement. Some patients experienced a decrease in pain as early as week 1, which persisted throughout the study.
^ Serotonin Syndrome
The development of a potentially life-threatening serotonin syndrome has been reported with SNRIs and SSRIs, including Duloxetine Delayed-release Capsules, alone but particularly with concomitant use of other serotonergic drugs (including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, and St. John's Wort) and with drugs that impair metabolism of serotonin (in particular, MAOIs, both those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue).
Serotonin syndrome symptoms may include mental status changes (e.g., agitation, hallucinations, delirium, and coma), autonomic instability (e.g., tachycardia, labile blood pressure, dizziness, diaphoresis, flushing, hyperthermia), neuromuscular symptoms (e.g., tremor, rigidity, myoclonus, hyperreflexia, incoordination), seizures, and/or gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea). Patients should be monitored for the emergence of serotonin syndrome.
The concomitant use of Duloxetine Delayed-release Capsules with MAOIs intended to treat psychiatric disorders is contraindicated. Duloxetine Delayed-release Capsules should also not be started in a patient who is being treated with MAOIs such as linezolid or intravenous methylene blue. All reports with methylene blue that provided information on the route of administration involved intravenous administration in the dose range of 1 mg/kg to 8 mg/kg. No reports involved the administration of methylene blue by other routes (such as oral tablets or local tissue injection) or at lower doses. There may be circumstances when it is necessary to initiate treatment with an MAOI such as linezolid or intravenous methylene blue in a patient taking Duloxetine Delayed-release Capsules. Duloxetine Delayed-release Capsules should be discontinued before initiating treatment with the MAOI [see Dosage and Administration (2.8, 2.9), and Contraindications (4)].
If concomitant use of Duloxetine Delayed-release Capsules with other serotonergic drugs including triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, buspirone, tryptophan and St. John's Wort is clinically warranted, patients should be made aware of a potential increased risk for serotonin syndrome, particularly during treatment initiation and dose increases. Treatment with Duloxetine Delayed-release Capsules and any concomitant serotonergic agents, should be discontinued immediately if the above events occur and supportive symptomatic treatment should be initiated.
^ Smoking Status
Duloxetine bioavailability (AUC) appears to be reduced by about one-third in smokers. Dosage modifications are not recommended for smokers.
^ Use Of Duloxetine Delayed-release Capsules With Other Maois Such As Linezolid Or Methylene Blue
Do not start Duloxetine Delayed-release Capsules in a patient who is being treated with linezolid or intravenous methylene blue because there is an increased risk of serotonin syndrome. In a patient who requires more urgent treatment of a psychiatric condition, other interventions, including hospitalization, should be considered [see Contraindications (4)].
In some cases, a patient already receiving Duloxetine Delayed-release Capsules therapy may require urgent treatment with linezolid or intravenous methylene blue. If acceptable alternatives to linezolid or intravenous methylene blue treatment are not available and the potential benefits of linezolid or intravenous methylene blue treatment are judged to outweigh the risks of serotonin syndrome in a particular patient, Duloxetine Delayed-release Capsules should be stopped promptly, and linezolid or intravenous methylene blue can be administered. The patient should be monitored for symptoms of serotonin syndrome for 5 days or until 24 hours after the last dose of linezolid or intravenous methylene blue, whichever comes first. Therapy with Duloxetine Delayed-release Capsules may be resumed 24 hours after the last dose of linezolid or intravenous methylene blue [see Warnings and Precautions (5.4)].
The risk of administering methylene blue by non-intravenous routes (such as oral tablets or by local injection) or in intravenous doses much lower than 1 mg/kg with Duloxetine Delayed-release Capsules is unclear. The clinician should, nevertheless, be aware of the possibility of emergent symptoms of serotonin syndrome with such use [see Warnings and Precautions (5.4)].
^ Race
No specific pharmacokinetic study was conducted to investigate the effects of race.
^ Drugs That Interfere With Hemostasis (e.g., Nsaids, Aspirin, And Warfarin)
Serotonin release by platelets plays an important role in hemostasis. Epidemiological studies of the case-control and cohort design that have demonstrated an association between use of psychotropic drugs that interfere with serotonin reuptake and the occurrence of upper gastrointestinal bleeding have also shown that concurrent use of an NSAID or aspirin may potentiate this risk of bleeding. Altered anticoagulant effects, including increased bleeding, have been reported when SSRIs or SNRIs are co-administered with warfarin. Concomitant administration of warfarin (2-9 mg once daily) under steady state conditions with duloxetine 60 or 120 mg once daily for up to 14 days in healthy subjects (n=15) did not significantly change INR from baseline (mean INR changes ranged from 0.05 to +0.07). The total warfarin (protein bound plus free drug) pharmacokinetics (AUCτ,ss, Cmax,ss or tmax,ss) for both R- and S-warfarin were not altered by duloxetine. Because of the potential effect of duloxetine on platelets, patients receiving warfarin therapy should be carefully monitored when duloxetine is initiated or discontinued [see Warnings and Precautions (5.5)].
^ Dosage For Treatment Of Diabetic Peripheral Neuropathic Pain
Administer Duloxetine Delayed-release Capsules 60 mg once daily. There is no evidence that doses higher than 60 mg confer additional significant benefit and the higher dose is clearly less well tolerated [see Clinical Studies (14.3)]. For patients for whom tolerability is a concern, a lower starting dose may be considered.
Since diabetes is frequently complicated by renal disease, consider a lower starting dose and gradual increase in dose for patients with renal impairment [see Dosage and Administration (2.6), Use in Specific Populations (8.10), and Clinical Pharmacology (12.3)].
^ Discontinuation Of Treatment With Duloxetine Delayed-release Capsules
Discontinuation symptoms have been systematically evaluated in patients taking duloxetine. Following abrupt or tapered discontinuation in adult placebo-controlled clinical trials, the following symptoms occurred at 1% or greater and at a significantly higher rate in duloxetine-treated patients compared to those discontinuing from placebo: dizziness, headache, nausea, diarrhea, paresthesia, irritability, vomiting, insomnia, anxiety, hyperhidrosis, and fatigue.
During marketing of other SSRIs and SNRIs (serotonin and norepinephrine reuptake inhibitors), there have been spontaneous reports of adverse events occurring upon discontinuation of these drugs, particularly when abrupt, including the following: dysphoric mood, irritability, agitation, dizziness, sensory disturbances (e.g., paresthesias such as electric shock sensations), anxiety, confusion, headache, lethargy, emotional lability, insomnia, hypomania, tinnitus, and seizures. Although these events are generally self-limiting, some have been reported to be severe.
Patients should be monitored for these symptoms when discontinuing treatment with Duloxetine Delayed-release Capsules. A gradual reduction in the dose rather than abrupt cessation is recommended whenever possible. If intolerable symptoms occur following a decrease in the dose or upon discontinuation of treatment, then resuming the previously prescribed dose may be considered. Subsequently, the physician may continue decreasing the dose but at a more gradual rate [see Dosage and Administration (2.7)].
^ Drugs Metabolized By Cyp2c9
Results of in vitro studies demonstrate that duloxetine does not inhibit activity. In a clinical study, the pharmacokinetics of S-warfarin, a CYP2C9 substrate, were not significantly affected by duloxetine [see Drug Interactions (7.4)].
^ Suicidal Thoughts And Behaviors In Children, Adolescents, And Young Adults
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment.
Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18-24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk of differences (drug vs placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 1.
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
If the decision has been made to discontinue treatment, medication should be tapered, as rapidly as is feasible, but with recognition that discontinuation can be associated with certain symptoms [see Dosage and Administration (2.7) and Warnings and Precautions (5.7) for descriptions of the risks of discontinuation of Duloxetine Delayed-release Capsules].
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to health care providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for Duloxetine Delayed-release Capsules should be written for the smallest quantity of capsules consistent with good patient management, in order to reduce the risk of overdose.
^ Lorazepam
Under steady-state conditions for duloxetine (60 mg Q 12 hours) and lorazepam (2 mg Q 12 hours), the pharmacokinetics of duloxetine were not affected by co-administration.
^ Severe Renal Impairment
Limited data are available on the effects of duloxetine in patients with end-stage renal disease (ESRD). After a single 60 mg dose of duloxetine, Cmax and AUC values were approximately 100% greater in patients with end-stage renal disease receiving chronic intermittent hemodialysis than in subjects with normal renal function. The elimination half-life, however, was similar in both groups. The AUCs of the major circulating metabolites, 4-hydroxy duloxetine glucuronide and 5-hydroxy, 6-methoxy duloxetine sulfate, largely excreted in urine, were approximately 7- to 9-fold higher and would be expected to increase further with multiple dosing. Population PK analyses suggest that mild to moderate degrees of renal impairment (estimated CrCl 30-80 mL/min) have no significant effect on duloxetine apparent clearance [see Dosage and Administration (2.6) and Warnings and Precautions (5.14)].
^ Management Of Overdose
There is no specific antidote to Duloxetine Delayed-release Capsules, but if serotonin syndrome ensues, specific treatment (such as with cyproheptadine and/or temperature control) may be considered. In case of acute overdose, treatment should consist of those general measures employed in the management of overdose with any drug.
An adequate airway, oxygenation, and ventilation should be assured, and cardiac rhythm and vital signs should be monitored. Induction of emesis is not recommended. Gastric lavage with a large-bore orogastric tube with appropriate airway protection, if needed, may be indicated if performed soon after ingestion or in symptomatic patients.
Activated charcoal may be useful in limiting absorption of duloxetine from the gastrointestinal tract. Administration of activated charcoal has been shown to decrease AUC and Cmax by an average of one-third, although some subjects had a limited effect of activated charcoal. Due to the large volume of distribution of this drug, forced diuresis, dialysis, hemoperfusion, and exchange transfusion are unlikely to be beneficial.
In managing overdose, the possibility of multiple drug involvement should be considered. A specific caution involves patients who are taking or have recently taken Duloxetine Delayed-release Capsules and might ingest excessive quantities of a TCA. In such a case, decreased clearance of the parent tricyclic and/or its active metabolite may increase the possibility of clinically significant sequelae and extend the time needed for close medical observation [see Warnings and Precautions (5.4) and Drug Interactions (7)]. The physician should consider contacting a poison control center (1-800-222-1222 or www.poison.org) for additional information on the treatment of any overdose. Telephone numbers for certified poison control centers are listed in the Physicians' Desk Reference (PDR).
^ Gender
Duloxetine's half-life is similar in men and women. Dosage adjustment based on gender is not necessary.
^ Pharmacokinetics
Duloxetine has an elimination half-life of about 12 hours (range 8 to 17 hours) and its pharmacokinetics are dose proportional over the therapeutic range. Steady-state plasma concentrations are typically achieved after 3 days of dosing. Elimination of duloxetine is mainly through hepatic metabolism involving two P450 isozymes, CYP1A2 and CYP2D6.
^ Effects On Male And Female Sexual Function In Adults
Changes in sexual desire, sexual performance and sexual satisfaction often occur as manifestations of psychiatric disorders or diabetes, but they may also be a consequence of pharmacologic treatment. Because adverse sexual reactions are presumed to be voluntarily underreported, the Arizona Sexual Experience Scale (ASEX), a validated measure designed to identify sexual side effects, was used prospectively in 4 MDD placebo-controlled trials. In these trials, as shown in Table 5 below, patients treated with Duloxetine Delayed-release Capsules experienced significantly more sexual dysfunction, as measured by the total score on the ASEX, than did patients treated with placebo. Gender analysis showed that this difference occurred only in males. Males treated with Duloxetine Delayed-release Capsules experienced more difficulty with ability to reach orgasm (ASEX Item 4) than males treated with placebo. Females did not experience more sexual dysfunction on Duloxetine Delayed-release Capsules than on placebo as measured by ASEX total score. Negative numbers signify an improvement from a baseline level of dysfunction, which is commonly seen in depressed patients. Physicians should routinely inquire about possible sexual side effects.
^ Drugs Highly Bound To Plasma Protein
Because duloxetine is highly bound to plasma protein, administration of Duloxetine Delayed-release Capsules to a patient taking another drug that is highly protein bound may cause increased free concentrations of the other drug, potentially resulting in adverse reactions. However, co-administration of duloxetine (60 or 120 mg) with warfarin (2-9 mg), a highly protein-bound drug, did not result in significant changes in INR and in the pharmacokinetics of either total S-or total R-warfarin (protein bound plus free drug) [see Drug Interactions (7.4)].
^ Mechanism Of Action
Although the exact mechanisms of the antidepressant, central pain inhibitory and anxiolytic actions of duloxetine in humans are unknown, these actions are believed to be related to its potentiation of serotonergic and noradrenergic activity in the CNS.
^ Other Adverse Reactions Observed During The Premarketing And Postmarketing Clinical Trial Evaluation Of Duloxetine In Adults
Following is a list of treatment-emergent adverse reactions reported by patients treated with duloxetine in clinical trials. In clinical trials of all indications, 34,756 patients were treated with duloxetine. Of these, 26.9% (9337) took duloxetine for at least 6 months, and 12.4% (4317) for at least one year. The following listing is not intended to include reactions (1) already listed in previous tables or elsewhere in labeling, (2) for which a drug cause was remote, (3) which were so general as to be uninformative, (4) which were not considered to have significant clinical implications, or (5) which occurred at a rate equal to or less than placebo.
Reactions are categorized by body system according to the following definitions: frequent adverse reactions are those occurring in at least 1/100 patients; infrequent adverse reactions are those occurring in 1/100 to 1/1000 patients; rare reactions are those occurring in fewer than 1/1000 patients.
Cardiac Disorders — Frequent: palpitations; Infrequent: myocardial infarction and tachycardia.
Ear and Labyrinth Disorders — Frequent: vertigo; Infrequent: ear pain and tinnitus.
Endocrine Disorders — Infrequent: hypothyroidism.
Eye Disorders — Frequent: vision blurred; Infrequent: diplopia, dry eye, and visual impairment.
Gastrointestinal Disorders — Frequent: flatulence; Infrequent: dysphagia, eructation, gastritis, gastrointestinal hemorrhage, halitosis, and stomatitis; Rare: gastric ulcer.
General Disorders and Administration Site Conditions — Frequent: chills/rigors; Infrequent: falls, feeling abnormal, feeling hot and/or cold, malaise, and thirst; Rare: gait disturbance.
Infections and Infestations — Infrequent: gastroenteritis and laryngitis.
Investigations — Frequent: weight increased, weight decreased; Infrequent: blood cholesterol increased.
Metabolism and Nutrition Disorders — Infrequent: dehydration and hyperlipidemia; Rare: dyslipidemia.
Musculoskeletal and Connective Tissue Disorders — Frequent: musculoskeletal pain; Infrequent: muscle tightness and muscle twitching.
Nervous System Disorders — Frequent: dysgeusia, lethargy, and paraesthesia/hypoesthesia; Infrequent: disturbance in attention, dyskinesia, myoclonus, and poor quality sleep; Rare: dysarthria.
Psychiatric Disorders — Frequent: abnormal dreams and sleep disorder; Infrequent: apathy, bruxism, disorientation/confusional state, irritability, mood swings, and suicide attempt; Rare: completed suicide.
Renal and Urinary Disorders — Frequent: urinary frequency; Infrequent: dysuria, micturition urgency, nocturia, polyuria, and urine odor abnormal.
Reproductive System and Breast Disorders — Frequent: anorgasmia/orgasm abnormal; Infrequent: menopausal symptoms, sexual dysfunction, and testicular pain; Rare: menstrual disorder.
Respiratory, Thoracic and Mediastinal Disorders — Frequent: yawning, oropharyngeal pain; Infrequent: throat tightness.
Skin and Subcutaneous Tissue Disorders — Frequent: pruritus; Infrequent: cold sweat, dermatitis contact, erythema, increased tendency to bruise, night sweats, and photosensitivity reaction; Rare: ecchymosis.
Vascular Disorders — Frequent: hot flush; Infrequent: flushing, orthostatic hypotension, and peripheral coldness.